Bệnh nhân nữ đã mổ cắt đĩa đệm trước đó, hiện đau theo rễ hai chi dưới.
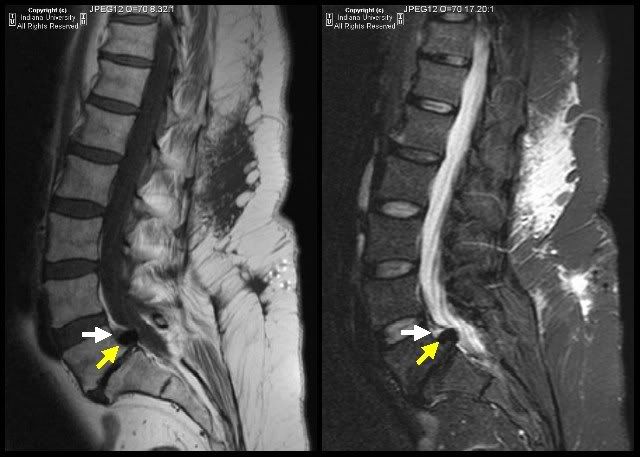
* MR:
- trượt trước độ I L5/S1
- khuyết eo L5 hai bên
- không thấy đĩa đệm trong khoảng gian đốt L5/S1
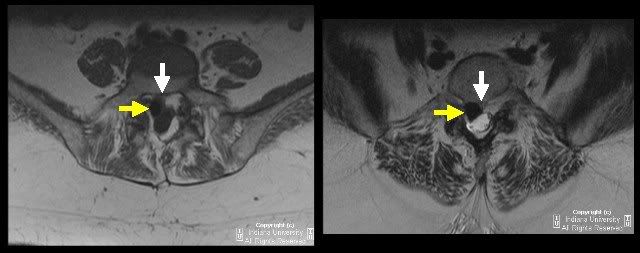
- tổn thương tròn (mũi tên vàng) phía sau L5 cạnh phải đường giữa với tín hiệu rất thấp trên mọi chuỗi xung
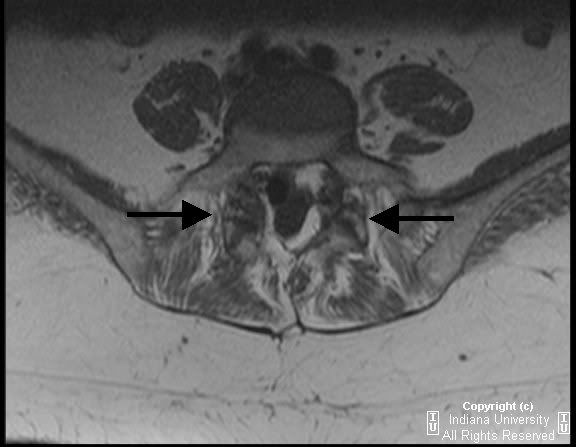
- trên hình axial, tổn thương này chèn ép bao màng cứng, gây hẹp hoàn toàn ngách bên bên (P), chèn ép rễ thần kinh S1(P)
- trên hình sagittal, một cấu trúc hình tam giác (mũi tên trắng) nằm ngay phía trên tổn thương tròn nêu trên, đồng tín hiệu trên T1W, tăng tín hiệu trên STIR
* Trên CT scan, tổn thương tròn sau L5 được xác định là có tỉ trọng của khí
* MR có gado (không đưa hình): Cấu trúc hình tam giác ở mũi tên trắng bắt thuốc tương phản đồng nhất
* Chẩn đoán: Bọt khí nitơ (mũi tên vàng) ngoài màng cứng gây hiệu ứng choán chỗ nặng trên bao màng cứng và chèn ép rễ thần kinh. Thoát vị đĩa đệm (extruded disc) nằm phía trên bọt khí.
Discussion
The intervertebral disc consists of the nucleus pulposus surrounded by the annulus fibrosis. The nucleus pulposus is located near the posterior end of the disc. With increasing age, the nucleus pulposus is replaced by fibrocartilage. Fissures start developing in the annulus which is anchored to the anterior and posterior longitudinal ligaments. Negative pressure exists within the cracks. This results in nitrogen gas coming out of solution with subsequent deposition in the intervertebral disc. This is referred to as vacuum phenomenon.
Vacuum phenomenon is just one of the entities related to spine degenerative changes. The pathophysiology of the degeneration revolves around water loss in the disc and decreased resilience of the disc tissues leading to disc height loss. A combination of degenerative changes allow the disc to bulge and then herniate. However, it is important to note that discs can herniate without significant degenerative disease. Other characteristics of degeneration include endplate destruction and osteophyte formation.
Initial management is usually conservative. Physical therapy, NSAIDS and spinal injections are used. If conservative treatment fails, surgery is a consideration.
Degenerative changes or degenerative changes accompanied by disc herniation can contribute to back pain and radiculopathy via various mechanisms. Degeneration can lead to spinal stenosis, nerve root compression, spondylolisthesis and retrolisthesis.
Low back pain due to degenerative disc disease affects men and women equally. Low back pain related to degenerative disc disease usually affects middle-age person. The typical peak is around 40 year of age.
Radiologic Overview:
MR is the study of choice to evaluate degenerative disc disease. Typically, sagittal T1 weighted, T2 weighted and STIR sequences are obtained. Axial T1 and T2 images are also obtained.
The foramen are assessed for bony constriction while making sure that the exiting nerve and adjacent fat is delineated on both axial and sagittal images. The central canal is evaluated for bony osteophytes contributing to stenosis. Spinal cord compression is usually readily identified. Disc height and desiccation is best evaluated on sagittal images. Alignment of the lumbar vertebral bodies is best evaluated on sagittal imaging. Annular tears will appear as bright spots on fluid sensitive sequences.
Herniation is localized displacement of disc material beyond the intervertebral disc space. Certain terminology is applied when describing disc related findings. On axial imaging, focal protrusion is used when there is displacement of less than 25% of the disc diameter. The term broad based is used when 25 to 50 % of the diameter is involved. If more than 50% of the diameter is involved, then the term diffuse bulge is used.
If the protruding disc material is inferiorly or superiorly displaced, then the term extrusion is used. If the disc material that is displaced is not in continuity with the parent disc, then the term sequestered disc fragment is used. Administration of contrast is important if there is a history of surgery to distinguish between scar and disc. Impingement by displaced disc on the thecal sac or the nerve roots is readily visualized using MR.
The bone marrow signal is usually evaluated using sagittal images. Endplate degenerative changes can be identified. Changes that are hypo intense on T1 and hyper intense on T2 are classified as Type 1. Type 2 changes are bright on T1 and T2. Type 1 changes are associated with subacute inflammatory changes while T2 changes are related to yellow marrow. Type 3 changes are hypo intense on T1 and T2. This is representative of sclerotic changes.
When myelogram is used, it is usually combined with CT. Given its invasive nature, this procedure it typically reserved for when MR and CT are unable to answer a question or when MR is contraindicated in a patient. Myelogram-CT is relied upon in cases where fine evaluation of uncovertebral joint disease in relation to nerve roots is warranted (typically the cervical spine). It also is helpful in spinal cord compression. Essentially, bony detail in degenerative disease is better evaluated using this procedure.
A conventional CT can be handy to evaluate bony detail of the spinal column. However, the degree of compression on the thecal sac and nerve roots by extradural bony lesions is better appreciated using MR or CT-myelogram. The spinal cord and soft tissues are better evaluated on MR.
Plain film radiography can be used to identify bony foraminal narrowing, intervertebral disc space narrowing, vacuum disc, osteophyte formation, and alignment. Plain films do not offer the same sensitivity offered by cross sectional imaging.
Key points:
- The intervertebral disc is composed of the nucleus pulposus surrounded by the annulus fibrosus.
- Vacuum disc phenomena is one of the findings associated with degenerative disc disease.
- Fissuring in the annulus creates spaces that become filled with nitrogen resulting in vacuum disc phenomena.
- Degenerative changes of the disc may lead to bulging and herniation.
- Degenerative changes along with disc herniation can cause spinal stenosis and nerve root compression.
- MRI of the lumbar spine is the modality of choice to evaluate for degenerative disc disease
- MRI helps evaluate for foraminal stenosis, central canal stenosis, spinal cord compression and nerve root compression
- Contrast administration is important to distinguish between post surgical scar and displaced disc.
- CT and/or CT myelogram can be used to evaluate patients in whom MRI is contraindicated.
- 90% of disc herniations are at L4-L5 or L5-S1
- Disc herniations are almost always confined to an extradural location
- Other considerations for an extradural spinal lesion include among others lymphoma, metastasis and neurofibroma.
References:
1. Grossman, R. Neuroradiology: The Requisites. Ch 16, Anatomy and Degenerative Diseases of the Spine.
2. Patel, R. Lumbar Degenerative Disc Disease. www.emedicine.com.


Không có nhận xét nào:
Đăng nhận xét